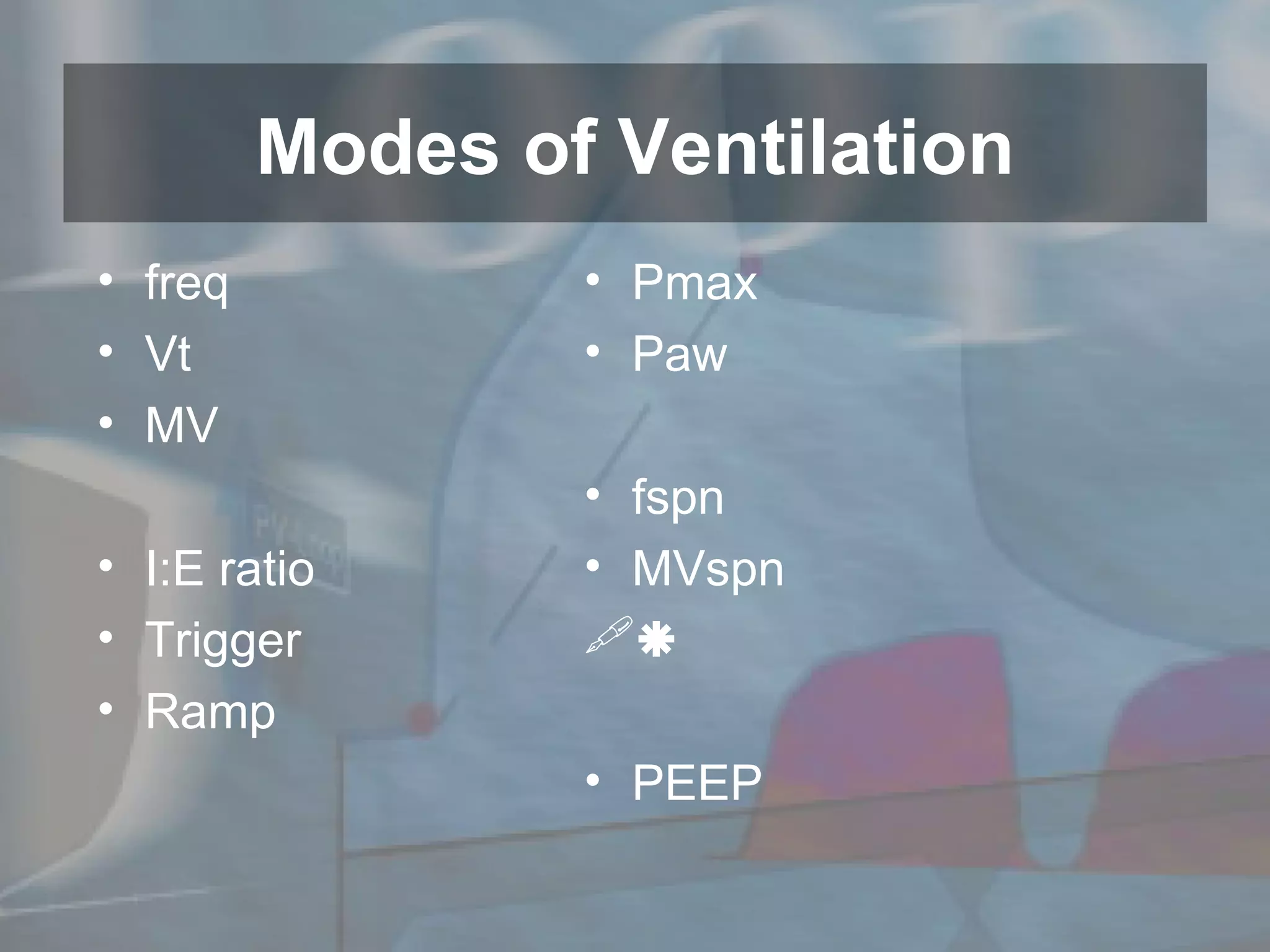
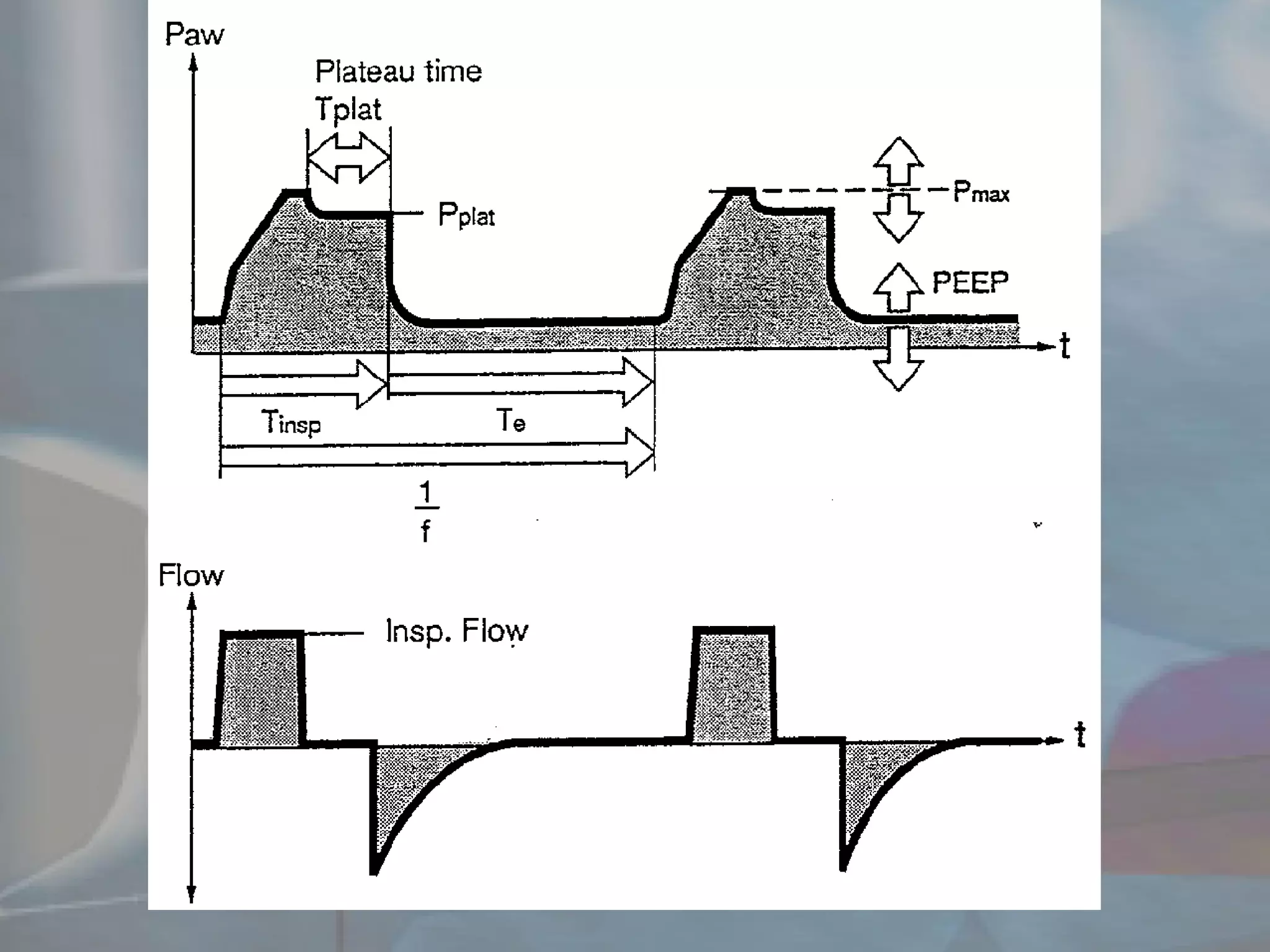
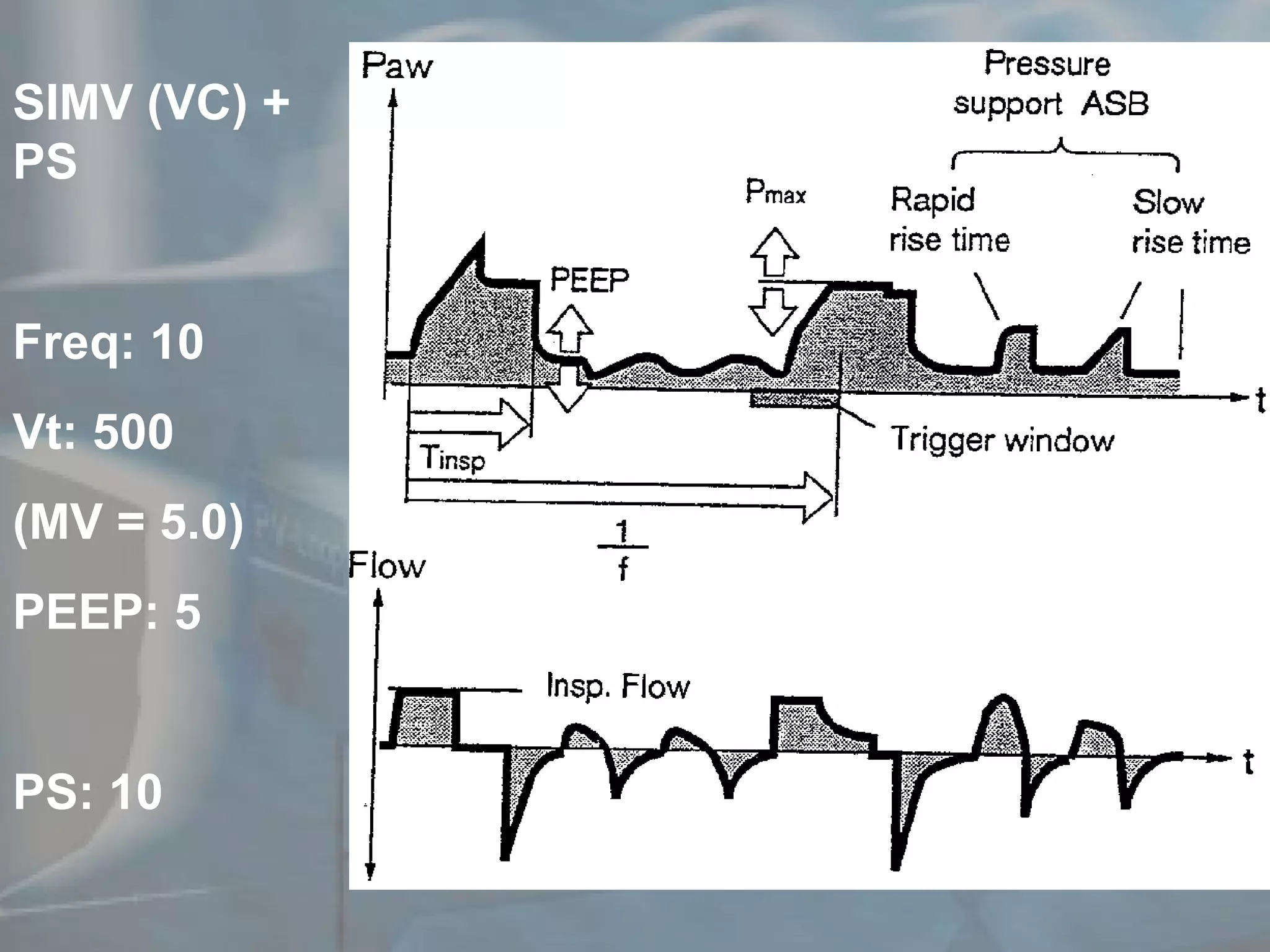
The document discusses principles of ventilation including indications for ventilation such as support through illness or reversal of hypoxemia. It describes modes of ventilation including controlled, pressure control, volume control, continuous positive airway pressure, and pressure support. It also discusses patient management considerations for ventilated patients such as monitoring, suctioning, sedation, positioning, nutrition, communication, and readiness to wean from ventilation. Complications of ventilation are also briefly outlined.